Dr Juan D. Cañete, from the Rheumatology Service at the Hospital Clínic and researcher in the IDIBAPS Inflammatory Joint Diseases (GRAI) group participated in this paper, coordinated by researchers from Friedrich-Alexander-University (FAU) Erlangen-Nürnberg and published in the journal ‘Nature Immunology’.
Rheumatoid arthritis is a chronic inflammatory autoimmune disease, which mainly affects the joints. It affects 1% of the global population and is more common in women. It is characterized by pain and inflammation in the small and large joints and, in more severe cases, eventually leads to joint destruction, which can cause disability and reduced life expectancy, if not treated properly.
Fibroblasts are cells found in connective tissue in the joints and they play an important role in regulating inflammation. They can be divided up into several subtypes, some of which promote inflammation and joint damage, whilst others have protective functions. “To date, it was not known whether fibroblasts changed their phenotype during the resolution of inflammation,” explains Dr. Juan D. Cañete.
The crucial role fibroblasts play in the resolution of inflammation
The study identified that CD200+ fibroblasts have pro-resolving properties and form a mesenchymal network, which not only regulates inflammation, but also promotes tissue repair. Using advanced sequencing and cell analysis techniques, the team characterized the specific functions of these fibroblasts in rheumatoid arthritis.
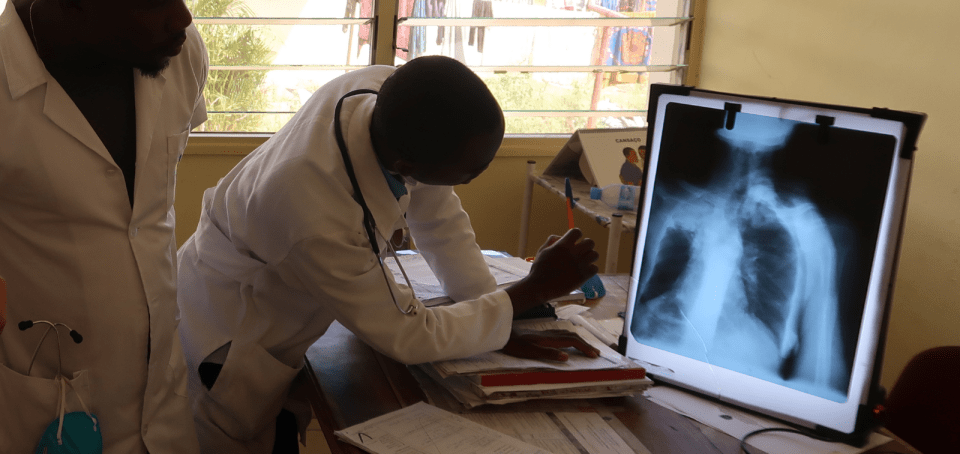
Using positron emission tomography (PET) with a fibroblast activation protein (FAP) inhibitor, the researchers visualized fibroblast activation in vivo for the first time. “The data revealed a fundamental activation of fibroblasts in the joints, entheses (connective tissue between soft tissue and bone), and the bones of patients with rheumatoid arthritis, psoriatic arthritis and axial spondyloarthritis, which was reversed by the therapeutic inhibition of cytokines (anti-TNF or anti-IL17A) during the resolution of the inflammation”, says Dr. Cañete.
On the other hand, single-cell transcriptomic and spatial transcriptomic analyses in experimental arthritis models showed that fibroblasts change phenotype from a pro-inflammatory to a pro-resolving type. They also showed that CD200+ fibroblasts interact with type 2 innate lymphoid cells and induce the resolution of inflammation, through the production of anti-inflammatory cytokines. CD200+ fibroblasts were also detected in patients with a non-inflammatory synovial micro-environment.
Modulating fibroblast activity
Researchers are now studying how CD200+ fibroblast activity can be modulated therapeutically, and how to find molecules or compounds to increase the quantity and activity of this cell type in affected joints.
At present, there are no therapies targeting fibroblasts for the treatment of chronic inflammatory diseases. The results of the study in Nature Immunology show that the administration of CD200-Fc, an experimental therapy that imitates the effects of pro-resolving fibroblasts, can control inflammation and tissue damage in arthritis. “CD200-Fc can provide a new therapeutic option to effectively promote a pro-resolving environment in joints and restore tissue homeostasis in arthritis”, concludes Dr. Cañete.
Thus, the results of the study demonstrate the prognostic utility of PET/CT with an FEP tracer in patients with chronic immune-mediated arthritis, by detecting pro-inflammatory fibroblast activity that is associated with bone destruction, and also open new therapeutic perspectives, not only in rheumatoid arthritis but also in other chronic inflammatory diseases.
Study reference:
Rauber S, Mohammadian H, Schmidkonz C, Atzinger A, Soare A, Treutlein C, Kemble S, Mahony CB, Geisthoff M, Angeli MR, Raimondo MG, Xu C, Yang KT, Lu L, Labinsky H, Saad MSA, Gwellem CA, Chang J, Huang K, Kampylafka E, Knitza J, Bilyy R, Distler JHW, Hanlon MM, Fearon U, Veale DJ, Roemer FW, Bäuerle T, Maric HM, Maschauer S, Ekici AB, Buckley CD, Croft AP, Kuwert T, Prante O, Cañete JD, Schett G, Ramming A. CD200+ fibroblasts form a pro-resolving mesenchymal network in arthritis. Nat Immunol. 2024 Apr;25(4):682-692. doi: 10.1038/s41590-024-01774-4.